Testicle Anatomy and Important clinical conditions
The testicles or testes are the main structures of the male reproductive system in bilateral orientation. These are similar structures to the female ovary with a few differences. In addition, testicles are present in the saccular structure, the scrotum, which is the extension of the abdominal wall anteriorly. This article summaries the keen details of testicle anatomy with proper illustration, focusing on different anatomical features. Let us look in detail to have a complete review of different aspects of testicle anatomy.
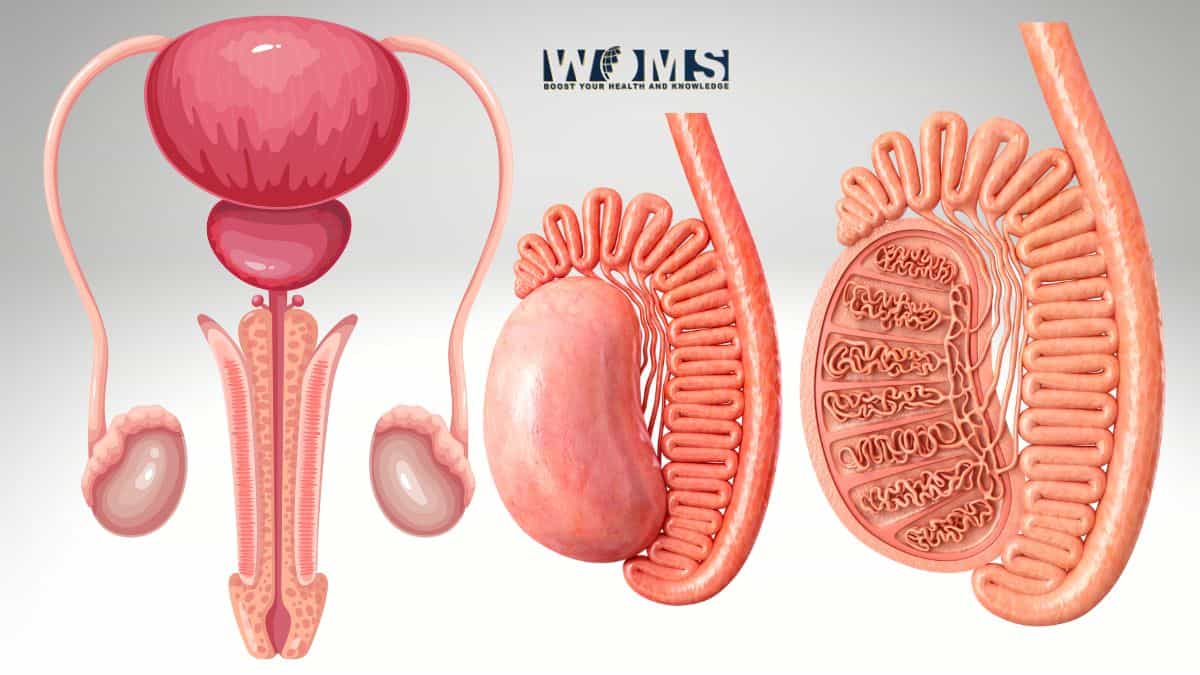
Structural orientation of testicle
In terms of testicle anatomy, they are ovoid in shape with a length of about 4-6cm. Testicles originate retroperitoneally along the posterior aspect of the abdominal wall. From this point, it moves in a downward direction up to the scrotum before the delivery of the baby. Moreover, the scrotum usually exhibits asymmetric representation with one testicle more downward in position than the other. These testicles usually remain in contact with the abdomen through a spermatic cord. Moreover, these are connected to the scrotum through the testicular ligament.
On the inner side of the scrotum, there are three layers that surround the testicles. These covers are moving from exterior to interior structures.
- External spermatic fascia – actually originates from the external oblique muscle of the anterior abdominal wall.
- Cremaster muscular layer – it originates from the internal oblique muscle of the anterior abdominal wall.
- Internal spermatic fascia – originates from the transversalis deep fascia of the anterior abdominal wall.
Moreover, there are also additional coverings surrounding the testicles from different aspects. Let us have a look at these layers to learn in detail about testicle anatomy.
- Tunica vaginalis – partially surrounds the testis, originating from the vaginal process. It needs to be mentioned while talking about testicle anatomy. It is further divided into the visceral and parietal layers.
- Visceral layer – surrounds the testicles, inferior portion of ductus deferens, and epididymis head
- Parietal layer – covers the superior aspect of the distal spermatic cord and duct of epididymis.
Physiologic features of the testicle
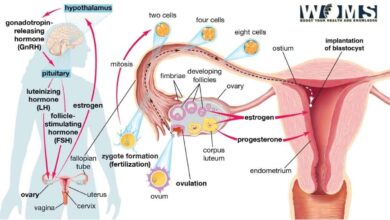
Along with testicle anatomy, let’s have a look at it’s physiological significance. The testicle performs the same function of producing sex hormones just like the female ovary. These sex hormones are also known as androgens, usually steroids in nature.
The most common hormone produced by the testicle is testosterone. In addition, these hormones are usually processed by a process known as steroidogenesis, the formation of steroids. All the processes of forming these sex hormones are best controlled by the anterior pituitary gland. There are two hormones that are released by the anterior pituitary gland, which indirectly or directly help to stimulate the production of sex hormones.
- Luteinizing hormone, produced by the anterior pituitary gland, controls the formation of testosterone.
- Follicle-stimulating hormone control and accelerates the process of sperm production.
Embryological aspects of testicle anatomy
As we mentioned in the testicle anatomy, the testicle develops retroperitoneally during intrauterine life. During the 26th week of pregnancy, the testicles continue descending towards the scrotum with the help of an inguinal cord. Testicles have their own neurovascular supply and lymphatic drainage present within the spermatic cord.
As testicles descend, they put a pushing pressure along the layers of the abdominal wall, and extend these structures to the scrotum. In this way, these extensions help to form a muscular pouch surrounding the testicles in the boundaries of the scrotum. Testicles continue to descend outside the body to meet the optimal pressure for spermatogenesis. If the testicles stop descending outside the body, it may affect the process of spermatogenesis leading to infertility.
Testicle anatomy in detail
Testicles, being ovoid, exhibit medial and lateral surfaces separated through anterior and posterior edges. Along the posterosuperior edge, there is a structure known as epididymis. Whereas, along the inferior surface, there is a scrotal ligament that connects the testicle to the lower surface of the scrotum. Testicles are surrounded by a capsule made up of dense fibrous connective tissue, known as tunica albuginea. In addition, this connective tissue divides the testicles into lobules through septa formation.
These lobules of the testis contain seminiferous tubules that move towards the mediastinum testis. Just before entering, they modify their orientation from convoluted to straight seminiferous tubules. These straight tubules connect with each other forming a collecting area, known as rete testis. Now in this detail of testicle anatomy, let’s have a look at the different layers of the testis, moving outside to inside.
- Skin → Dartos fascia→ External spermatic fascia → Cremaster muscular layer → Internal spermatic fascia → Parietal tunica vaginalis→ Visceral tunica vaginalis → Tunica albuginea
Histological aspects of testicle anatomy
The tubular structure of the testicles is lined by stromal cells containing testosterone-containing interstitial or Leydig cells. In addition, these tubules are also lined with seminiferous epithelium containing Sertoli cells and sperm-forming cells. These sperm forms continue to multiply during the different phases of spermatogenesis. Moreover, Sertoli cells nourish these cells properly.
Blood supply of testicle
The major arterial blood supply of testis is through the testicular arteries, which are paired too. As these arteries are important, they need a special mention while discussing testicle anatomy. Testicular arteries originate from the abdominal aorta at the lower level of the renal artery. These arteries move towards the scrotum through the inguinal canal present in the spermatic cord. Moreover, the testicles also receive an additional blood supply through the cremasteric artery and the artery to the vas deferens. These collateral arterial branches play the main role during the obstruction of testicular arteries.
On the other hand, testes drain deoxygenated blood through the spermatic veins. These veins interlink with each other to form pampiniform plexus to drain deoxygenated blood from the testicles. Moreover, this plexus covers the branches of testicular arteries to maintain optimum temperature. These small veins join to form the main testicular vein to drain deoxygenated blood.
The right testicular vein directly drains deoxygenated blood into the inferior vena cava. Whereas, the left testicular vein empties into the renal vein.
Lymphatic drainage
Testicles drain lymph into the following lymph nodes.
- Pre-aortic
- Lateral-aortic
Nerve supply of testicle
Testicles receive their nerve supply through the autonomic nerve fibers. In this way, the testicles get innervated through the testicular plexus. This nerve plexus supplies the testis through the spermatic cord. The innervation of testicle is a must know while discussing testicle anatomy.
Clinical significance of testicle
- Testicles are a very sensitive structure of the male reproductive system. They can easily get injured through any contact injury. Pain from the testis can usually transfer to the abdominal cavity through the spermatic plexus. It may cause pain in the hip and back region, diminishing after a few minutes.
- Testicular torsion is an emergency condition to treat immediately. As it may cause ischemia in this region. If not treated surgically, there is a high chance that the testicle may be lost.
- Varicocele – is a medical condition exhibiting swollen veins of the testis. There is a higher prevalence of varicocele on the left side.
- Hydrocele testis – is caused by the collection of liquid around the testicles. It may cause scrotal swelling.
- Spermatocele – it is a retention cyst of the tubule of any male reproductive structure with watery liquids containing spermatozoa.
- Bell-clapper deformity – in this condition, testis are not attached to the scrotal walls. This type of testicle increases the risk of testicular torsion.
- Blue balls – it is a medical condition associated with fluid congestion in the testicles. This happens due to increased sexual arousal.
Frequently asked questions (FAQs)
What are the most common problems associated with testicles?
The most common disorders that may affect the function of testicles are as follows:
● Testicular torsion
● Hydrocele
● Testicular pain
Which testicle is usually on a lower level as compared to the other?
More often, the right testicle is larger than the left testicle. That’s why the left testicle is placed at a lower level than the right testicle.