How Smarter Manufacturing Can Bring Gene Therapies to More Patients
Gene and cell therapies are redefining modern medicine, offering curative potential for genetic and oncologic diseases once deemed untreatable. Yet their clinical success depends as much on manufacturing as on molecular design. Viral vectors, the biological vehicles delivering therapeutic DNA, remain difficult and expensive to produce. Despite major advances, yields are inconsistent, purification is inefficient, and manufacturing costs restrict patient access. This article explores the main bottlenecks in viral vector production, including upstream yields, downstream recovery, and analytical complexity, and examines how new process technologies, from intensified bioreactors to continuous purification and real-time analytics, are reshaping the economics and accessibility of advanced therapies.
When science meets manufacturing
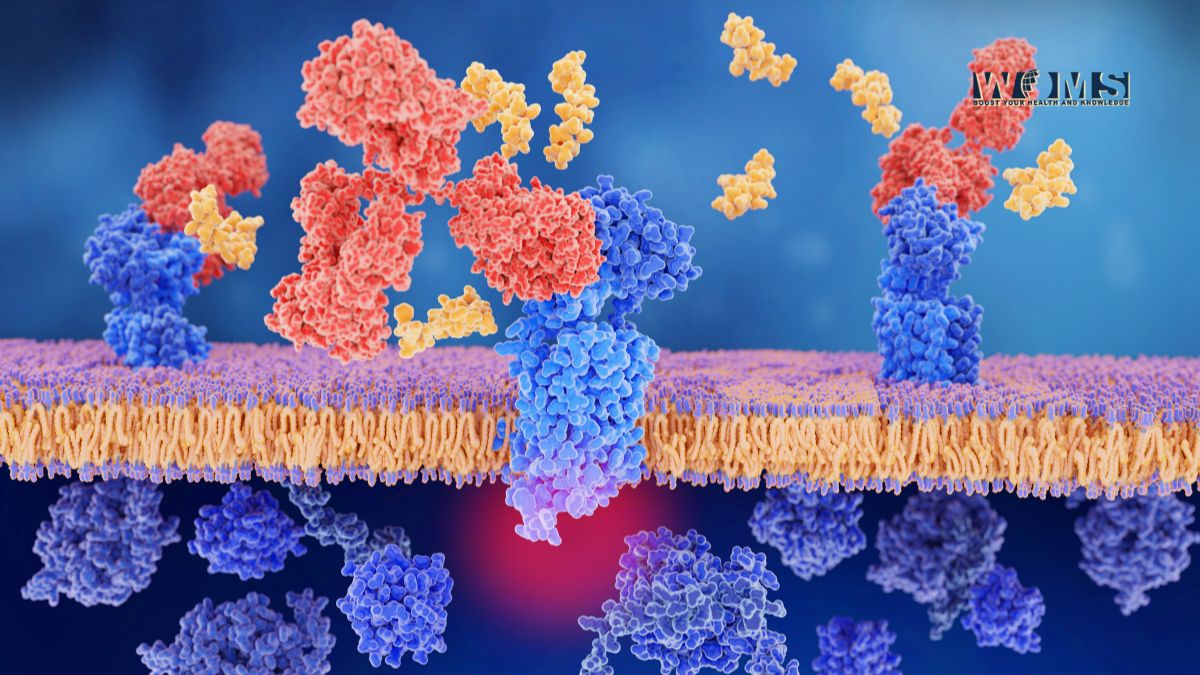
The past decade has turned gene therapy from a futuristic idea into clinical reality. Treatments using adeno-associated viruses (AAV), lentiviruses, and retroviruses are now approved for conditions such as spinal muscular atrophy, inherited retinal disease, and leukemia. These therapies can repair defective genes or equip immune cells with new abilities to fight cancer.
But each dose represents the product of an extraordinarily complex bioprocess. Billions of viral particles must be created, purified, tested, and filled under sterile, reproducible conditions, all within the limits of cost and quality imposed by regulatory agencies. Manufacturing has therefore become the true gatekeeper between medical innovation and patient availability.
Upstream: The productivity paradox
Upstream processing, the stage where viral vectors are generated within living cells, has evolved rapidly. Using optimized media and transient transfection systems, scientists can now achieve titers exceeding 10¹³ vector genomes per liter, compared to 10¹¹ just a decade ago.
Still, higher titers have not solved the cost problem. Scaling up from small laboratory vessels to 200-liter bioreactors introduces new inefficiencies. Gradients in pH, oxygen, and nutrient availability can alter viral quality and yield. Transfection itself remains inconsistent, relying on delicate plasmid-to-reagent ratios and transient gene expression that fluctuates from batch to batch.
Each lost percentage point in yield translates directly into higher cost per dose, a crucial metric when manufacturing a therapy that can cost over one million dollars per patient.
Downstream: The purification bottleneck
Once the viral particles are produced, the real challenge begins: purification. This phase, known as downstream processing, separates functional, full viral particles from host-cell debris, DNA, proteins, and empty shells.
Multiple filtration and chromatography steps are typically required to achieve clinical-grade purity. Each step removes contaminants but also sacrifices viral yield, often leaving only half of the produced material usable. For AAV, the separation of empty versus full capsids remains a persistent challenge; even small imbalances can impact potency and immune response.
Beyond purification, quality control adds weeks to production timelines. Analytical assays for potency, infectivity, and genome integrity are labor-intensive and slow. This means a batch can be produced in days but released only after months, delaying treatment schedules and inflating manufacturing costs.
Not all manufacturing obstacles are visible on the surface. One of the most common traps is process mismatch, when upstream production capacity outpaces downstream purification capabilities. A bioreactor might deliver a successful run, but if the purification train cannot process that volume efficiently, the material degrades or is lost.
Another hidden bottleneck lies in analytics. Incomplete or slow testing prevents real-time decision-making, so deviations go unnoticed until a batch fails later in the pipeline. The lack of rapid, validated assays for viral potency is one of the field’s largest blind spots.
These problems directly affect Cost of Goods (CoGs), where upstream yield (how much is made) and downstream recovery (how much survives purification) define economic viability. Small gains in recovery can cut total manufacturing cost by 20–30 %, underscoring why process control is not just technical, it is clinical.
Emerging technologies closing the gap
The next generation of bioprocess technologies is targeting these weak points directly.
Fixed-bed bioreactors, for instance, increase cell density dramatically without expanding footprint. Instead of relying on larger tanks, intensification allows more virus to be produced in smaller, closed systems. Perfusion cultures continuously feed fresh medium and remove waste, keeping cells productive for longer periods and boosting volumetric yields.
Continuous purification technologies are revolutionizing downstream workflows. Unlike traditional chromatography, which operates in discrete cycles, continuous systems maintain a steady-state flow. Column-free approaches such as Countercurrent Tangential Chromatography (CCTC) enable high recovery and consistent purity while minimizing resin usage and turnaround times.
These innovations are more than engineering upgrades, they represent a conceptual shift toward seamless, connected manufacturing pipelines.
Integration: Where technology becomes transformation
Technological improvements only achieve impact when they work together. Integration across upstream, downstream, and analytics is essential.
For example, intensified fixed-bed systems can now be paired with continuous chromatography in a single, closed manufacturing loop. This integration minimizes hold times, reduces contamination risk, and improves reproducibility. Some biomanufacturers, including leading European technology developers, are demonstrating how such hybrid systems can reshape the economics of gene therapy production.
Real-time monitoring further enhances control. Process Analytical Technology (PAT) tools track metabolites, pH, oxygen, and vector quality indicators directly inside the bioreactor. Combined with digital twins — virtual models that simulate and predict process behavior, these tools allow proactive adjustments rather than reactive troubleshooting. The result is shorter development timelines, fewer failed runs, and stronger regulatory confidence.
Why it matters for patients
Every improvement in manufacturing ripples outward to patient care. Higher yields and recoveries mean more doses from the same production run. Faster analytics shorten release cycles, ensuring timely treatment for conditions where delay can mean irreversible progression.
Reducing variability also builds trust. Consistent manufacturing quality underpins regulatory approval, and regulators now expect a clear understanding of process design space, the defined parameters where a process remains robust. Establishing this early enables faster scale-up, smoother tech transfer, and ultimately faster access for patients worldwide.
In resource-limited settings, these advances could make local production feasible, replacing dependency on imported gene therapies with regional manufacturing hubs. For diseases like hemophilia or rare immunodeficiencies, that could mean the difference between access and exclusion.
The human dimension of cost efficiency
Manufacturing may sound mechanical, but its consequences are human. When process inefficiencies inflate therapy prices, insurers restrict coverage, and patients wait. Streamlining production is therefore not just a technical necessity but a moral one. The global community faces the task of translating curative science into sustainable healthcare. Reducing cost of goods by even a fraction can free resources for new indications, improved logistics, and expanded patient inclusion.
Process modeling and economic simulations, used increasingly during early development, now allow scientists to forecast not only yield but financial feasibility, guiding investment and regulatory strategy simultaneously.
The path forward
Solving viral vector manufacturing bottlenecks requires convergence across disciplines.
Biologists must design constructs that fold and package efficiently. Engineers must refine intensified and continuous platforms for reproducibility. Data scientists must integrate real-time monitoring with predictive modeling. And regulators must support adaptive validation frameworks that keep pace with innovation.
The result will be a new manufacturing paradigm: smaller, smarter, and globally deployable. A future where a patient’s genetic medicine can be produced not in years but in weeks by better reproducibility, affordability, and safety.
The bottlenecks that once limited gene therapy are becoming the very blueprints for its next leap forward. When biology and engineering finally move in harmony, manufacturing will cease to be a barrier and become the bridge between discovery and cure.




